Vascular Response to Spreading Depolarization Predicts Stroke Outcome
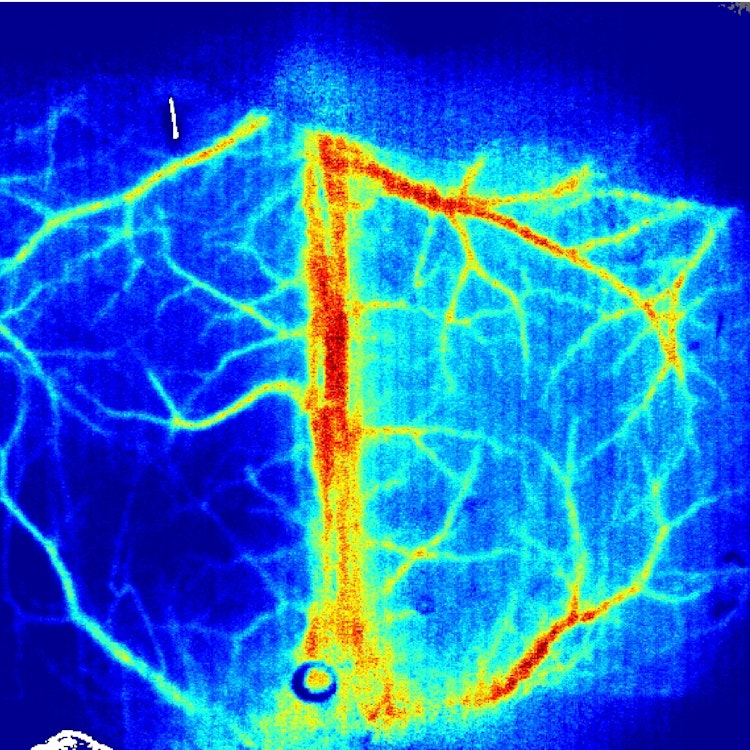
Background: Cortical spreading depolarization (CSD) is a massive neuro-glial depolarization wave, which propagates across the cerebral cortex. In stroke, CSD is a necessary and ubiquitous mechanism for the development of neuronal lesions that initiates in the ischemic core and propagates through the penumbra extending the tissue injury. Although CSD propagation induces dramatic changes in cerebral blood flow, the vascular responses in different ischemic regions and their consequences on reperfusion and recovery remain to be defined. Methods: Ischemia was performed using the thrombin model of stroke and reperfusion was induced by r-tPA (recombinant tissue-type plasminogen activator) administration in mice. We used in vivo electrophysiology and laser speckle contrast imaging simultaneously to assess both electrophysiological and hemodynamic characteristics of CSD after ischemia onset. Neurological deficits were assessed on day 1, 3, and 7. Furthermore, infarct sizes were quantified using 2,3,5-triphenyltetrazolium chloride on day 7. Results: After ischemia, CSDs were evidenced by the characteristic propagating DC shift extending far beyond the ischemic area. On the vascular level, we observed 2 types of responses: some mice showed spreading hyperemia confined to the penumbra area (penumbral spreading hyperemia) while other showed spreading hyperemia propagating in the full hemisphere (full hemisphere spreading hyperemia). Penumbral spreading hyperemia was associated with severe stroke-induced damage, while full hemisphere spreading hyperemia indicated beneficial infarct outcome and potential viability of the infarct core. In all animals, thrombolysis with r-tPA modified the shape of the vascular response to CSD and reduced lesion volume. Conclusions: Our results show that different types of spreading hyperemia occur spontaneously after the onset of ischemia. Depending on their shape and distribution, they predict severity of injury and outcome. Furthermore, our data show that modulating the hemodynamic response to CSD may be a promising therapeutic strategy to attenuate stroke outcome.
Download
binder_2022.pdfResearchers






